Jha, V. et al. Chronic kidney disease: global dimension and perspectives. Lancet 382, 260–272 (2013).
Xie, Y. et al. Analysis of the Global Burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 94, 567–581 (2018).
Daratha, K. B. et al. Risks of subsequent hospitalization and death in patients with kidney disease. Clin. J. Am. Soc. Nephrol. 7, 409–416 (2012).
Klarenbach, S. W., Tonelli, M., Chui, B. & Manns, B. J. Economic evaluation of dialysis therapies. Nat. Rev. Nephrol. 10, 644–652 (2014).
Allen, R. P. et al. Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria — history, rationale, description, and significance. Sleep. Med. 15, 860–873 (2014).
AASM Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep 22, 667–689 (1999).
Montplaisir, J. et al. Clinical, polysomnographic, and genetic characteristics of restless legs syndrome: a study of 133 patients diagnosed with new standard criteria. Mov. Disord. 12, 61–65 (1997).
Doan, T. T., Koo, B. B., Ogilvie, R. P., Redline, S. & Lutsey, P. L. Restless legs syndrome and periodic limb movements during sleep in the Multi-Ethnic Study of Atherosclerosis. Sleep 41, zsy106 (2018).
Allen, R. P. et al. Restless legs syndrome prevalence and impact: REST general population study. Arch. Intern. Med. 165, 1286–1292, (2005).
Winkelman, J. W., Chertow, G. M. & Lazarus, J. M. Restless legs syndrome in end-stage renal disease. Am. J. Kidney Dis. 28, 372–378 (1996).
Hui, D. S. et al. Prevalence of sleep disturbances in Chinese patients with end-stage renal failure on continuous ambulatory peritoneal dialysis. Am. J. Kidney Dis. 36, 783–788 (2000).
Walker, S., Fine, A. & Kryger, M. H. Sleep complaints are common in a dialysis unit. Am. J. Kidney Dis. 26, 751–756 (1995).
Markou, N. et al. Sleep-disordered breathing in nondialyzed patients with chronic renal failure. Lung 184, 43–49 (2006).
Losso, R. L., Minhoto, G. R. & Riella, M. C. Sleep disorders in patients with end-stage renal disease undergoing dialysis: comparison between hemodialysis, continuous ambulatory peritoneal dialysis and automated peritoneal dialysis. Int. Urol. Nephrol. 47, 369–375 (2015).
Chrastina, M. et al. Impact of kidney transplantation on restless legs syndrome. Bratisl. Lek. Listy 116, 404–407 (2015).
Azar, S. A., Hatefi, R. & Talebi, M. Evaluation of effect of renal transplantation in treatment of restless legs syndrome. Transpl. Proc. 39, 1132–1133 (2007).
Allen, R. P., Auerbach, S., Bahrain, H., Auerbach, M. & Earley, C. J. The prevalence and impact of restless legs syndrome on patients with iron deficiency anemia. Am. J. Hematol. 88, 261–264 (2013).
Panwar, B. & Gutiérrez, O. M. Disorders of iron metabolism and anemia in chronic kidney disease. Semin. Nephrol. 36, 252–261 (2016).
Fishbane, S., Pollack, S., Feldman, H. I. & Joffe, M. M. Iron indices in chronic kidney disease in the National Health and Nutritional Examination Survey 1988–2004. Clin. J. Am. Soc. Nephrol. 4, 57–61 (2009).
Allen, R. P., Barker, P. B., Wehrl, F. W., Song, H. K. & Earley, C. J. MRI measurement of brain iron in patients with restless legs syndrome. Neurology 56, 263–265 (2001).
Jiménez-Jiménez, F. J., Alonso-Navarro, H., García-Martín, E. & Agúndez, J. A. G. Association between restless legs syndrome and peripheral neuropathy: a systematic review and meta-analysis. Eur. J. Neurol. 28, 2423–2442 (2021).
Jurcić, D. et al. Clinical course of uremic neuropathy in long-term hemodialysis. Coll. Antropol. 32, 771–775 (2008).
Mucsi, I. et al. Restless legs syndrome, insomnia and quality of life in patients on maintenance dialysis. Nephrol. Dial. Transpl. 20, 571–577 (2005).
Unruh, M. L. et al. Restless legs symptoms among incident dialysis patients: association with lower quality of life and shorter survival. Am. J. Kidney Dis. 43, 900–909 (2004).
Happe, S. et al. Assessing health-related quality of life in patients with restless legs syndrome. Sleep. Med. 10, 295–305 (2009).
Szentkiralyi, A. et al. Association between restless legs syndrome and depression in patients with chronic kidney disease. J. Psychosom. Res. 67, 173–180 (2009).
Benz, R. L., Pressman, M. R., Hovick, E. T. & Peterson, D. D. Potential novel predictors of mortality in end-stage renal disease patients with sleep disorders. Am. J. Kidney Dis. 35, 1052–1060 (2000).
Baiardi, S., Mondini, S., Baldi Antognini, A., Santoro, A. & Cirignotta, F. Survival of dialysis patients with restless legs syndrome: a 15-year follow-up study. Am. J. Nephrol. 46, 224–230 (2017).
Mirbagher Ajorpaz, N., Rahemi, Z., Aghajani, M. & Hashemi, S. H. Effects of glycerin oil and lavender oil massages on hemodialysis patients’ restless legs syndrome. J. Bodyw. Mov. Ther. 24, 88–92 (2020).
Oshvandi, K., Mirzajani Letomi, F., Soltanian, A. R. & Shamsizadeh, M. The effects of foot massage on hemodialysis patients’ sleep quality and restless leg syndrome: a comparison of lavender and sweet orange essential oil topical application. J. Complement. Integr. Med. 18, 843–850 (2021).
Chen, J. J. et al. Pharmacological and non-pharmacological treatments for restless legs syndrome in end-stage kidney disease: a systematic review and component network meta-analysis. Nephrol. Dial. Transpl. 37, 1982–1992 (2022).
Kashani, E., Mirhosseini, Z., Rastaghi, S. & Rad, M. The effect of the cool dialysate on the restless leg syndrome in hemodialysis patients: randomized triple-blind clinical trial. Iran. J. Nurs. Midwifery Res. 24, 200–205, (2019).
Palmieri-Smith, R. M., Leonard-Frye, J. L., Garrison, C. J., Weltman, A. & Ingersoll, C. D. Peripheral joint cooling increases spinal reflex excitability and serum norepinephrine. Int. J. Neurosci. 117, 229–242 (2007).
Huang, C. W. et al. Comparative efficacy and acceptability of treatments for restless legs syndrome in end-stage renal disease: a systematic review and network meta-analysis. Nephrol. Dial. Transpl. 35, 1609–1618 (2020).
Razazian, N., Azimi, H., Heidarnejadian, J., Afshari, D. & Ghadami, M. R. Gabapentin versus levodopa-c for the treatment of restless legs syndrome in hemodialysis patients: a randomized clinical trial. Saudi J. Kidney Dis. Transpl. 26, 271–278, (2015).
Dauvilliers, Y. et al. Rotigotine in hemodialysis-associated restless legs syndrome: a randomized controlled trial. Am. J. Kidney Dis. 68, 434–443 (2016).
Chincholkar, M. Gabapentinoids: pharmacokinetics, pharmacodynamics and considerations for clinical practice. Br. J. Pain. 14, 104–114 (2020).
Thorp, M. L., Morris, C. D. & Bagby, S. P. A crossover study of gabapentin in treatment of restless legs syndrome among hemodialysis patients. Am. J. Kidney Dis. 38, 104–108 (2001).
Micozkadioglu, H. et al. Gabapentin versus levodopa for the treatment of Restless Legs Syndrome in hemodialysis patients: an open-label study. Ren. Fail. 26, 393–397 (2004).
Collister, D. et al. The DIalysis Symptom COntrol-Restless Legs Syndrome (DISCO-RLS) Trial: a protocol for a randomized, crossover, placebo-controlled blinded trial. Can. J. Kidney Health Dis. 7, 2054358120968959 (2020).
Deng, Y., Wu, J. & Jia, Q. Efficacy of intravenous iron sucrose in hemodialysis patients with restless legs syndrome (RLS): a randomized, placebo-controlled study. Med. Sci. Monit. 23, 1254–1260 (2017).
Sloand, J. A., Shelly, M. A., Feigin, A., Bernstein, P. & Monk, R. D. A double-blind, placebo-controlled trial of intravenous iron dextran therapy in patients with ESRD and restless legs syndrome. Am. J. Kidney Dis. 43, 663–670 (2004).
Nyhuis, C. C. & Fernandez-Mendoza, J. Insomnia nosology: a systematic review and critical appraisal of historical diagnostic categories and current phenotypes. J. Sleep Res. 32, e13910 (2023).
Buysse, D. J., Reynolds, C. F. III, Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213 (1989).
Bastien, C. H., Vallières, A. & Morin, C. M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep. Med. 2, 297–307 (2001).
Sabbatini, M. et al. Insomnia in maintenance haemodialysis patients. Nephrol. Dial. Transpl. 17, 852–856 (2002).
Iliescu, E. A. et al. Quality of sleep and health-related quality of life in haemodialysis patients. Nephrol. Dial. Transpl. 18, 126–132 (2003).
Tu, C. Y., Chou, Y. H., Lin, Y. H. & Huang, W. L. Sleep and emotional disturbance in patients with non-dialysis chronic kidney disease. J. Formos. Med. Assoc. 118, 986–994 (2019).
Gislason, T. & Almqvist, M. Somatic diseases and sleep complaints. An epidemiological study of 3,201 Swedish men. Acta Med. Scand. 221, 475–481 (1987).
Bhaskar, S., Hemavathy, D. & Prasad, S. Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. J. Fam. Med. Prim. Care 5, 780–784, (2016).
Unruh, M. L. et al. Subjective and objective sleep quality in patients on conventional thrice-weekly hemodialysis: comparison with matched controls from the Sleep Heart Health Study. Am. J. Kidney Dis. 52, 305–313 (2008).
Parker, K. P., Kutner, N. G., Bliwise, D. L., Bailey, J. L. & Rye, D. B. Nocturnal sleep, daytime sleepiness, and quality of life in stable patients on hemodialysis. Health Qual. Life Outcomes 1, 68 (2003).
Pierratos, A. & Hanly, P. J. Sleep disorders over the full range of chronic kidney disease. Blood Purif. 31, 146–150 (2011).
Pérgola, P. E., Habiba, N. M. & Johnson, J. M. Body temperature regulation during hemodialysis in long-term patients: is it time to change dialysate temperature prescription? Am. J. Kidney Dis. 44, 155–165 (2004).
Te Lindert, B. H. W. & Van Someren, E. J. W. Skin temperature, sleep, and vigilance. Handb. Clin. Neurol. 156, 353–365 (2018).
Elder, S. J. et al. Sleep quality predicts quality of life and mortality risk in haemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol. Dial. Transpl. 23, 998–1004 (2008).
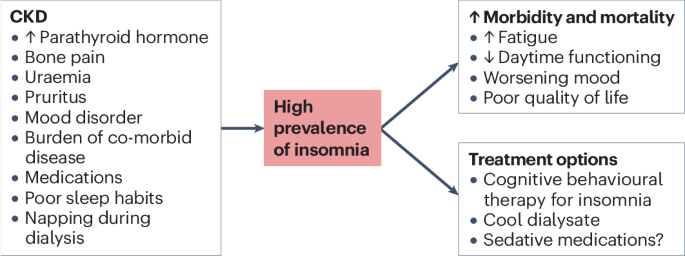
Lindner, A. V., Novak, M., Bohra, M. & Mucsi, I. Insomnia in patients with chronic kidney disease. Semin. Nephrol. 35, 359–372 (2015).
Hanly, P. J. & Pierratos, A. Improvement of sleep apnea in patients with chronic renal failure who undergo nocturnal hemodialysis. N. Engl. J. Med. 344, 102–107 (2001).
Loewen, A., Siemens, A. & Hanly, P. Sleep disruption in patients with sleep apnea and end-stage renal disease. J. Clin. Sleep. Med. 5, 324–329 (2009).
Beaudin, A. E. et al. Association of insomnia and short sleep duration, alone or with comorbid obstructive sleep apnea, and the risk of chronic kidney disease. Sleep 45, zsac088 (2022).
Wickwire, E. M., Juday, T. R., Gor, D., Amari, D. T. & Frech, F. H. Benzodiazepine usage, healthcare resource utilization, and costs among older adults treated with common insomnia medications: a retrospective cohort study. Clinicoecon Outcomes Res. 15, 413–424 (2023).
Díaz-Gutiérrez, M. J. et al. Relationship between the use of benzodiazepines and falls in older adults: a systematic review. Maturitas 101, 17–22 (2017).
Stewart, S. A. The effects of benzodiazepines on cognition. J. Clin. Psychiatry 66, 9–13 (2005).
Edinger, J. D. et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline. J. Clin. Sleep. Med. 17, 255–262 (2021).
Thomas, A. et al. Where are the behavioral sleep medicine providers and where are they needed? A geographic assessment. Behav. Sleep. Med. 14, 687–698 (2016).
Jacobs, G. D., Pace-Schott, E. F., Stickgold, R. & Otto, M. W. Cognitive behavior therapy and pharmacotherapy for insomnia: a randomized controlled trial and direct comparison. Arch. Intern. Med. 164, 1888–1896, (2004).
Montgomery, P. & Dennis, J. Cognitive behavioural interventions for sleep problems in adults aged 60+. Cochrane Database Syst. Rev. 2003, CD003161 (2003).
Chen, H. Y. et al. Cognitive-behavioral therapy for sleep disturbance in patients undergoing peritoneal dialysis: a pilot randomized controlled trial. Am. J. Kidney Dis. 52, 314–323 (2008).
Novak, M. J., Sheth, H., Bender, F. H., Fried, L. & Piraino, B. Improvement in Pittsburgh Symptom Score index after initiation of peritoneal dialysis. Adv. Perit. Dial. 24, 46–50 (2008).
Parker, K. P., Bailey, J. L., Rye, D. B., Bliwise, D. L. & Van Someren, E. J. Insomnia on dialysis nights: the beneficial effects of cool dialysate. J. Nephrol. 21, S71–S77 (2008).
Parker, K. P., Bailey, J. L., Rye, D. B., Bliwise, D. L. & Van Someren, E. J. Lowering dialysate temperature improves sleep and alters nocturnal skin temperature in patients on chronic hemodialysis. J. Sleep. Res. 16, 42–50 (2007).
Yumino, D. & Bradley, T. D. Central sleep apnea and Cheyne-Stokes respiration. Proc. Am. Thorac. Soc. 5, 226–236 (2008).
Jordan, A. S., McSharry, D. G. & Malhotra, A. Adult obstructive sleep apnoea. Lancet 383, 736–747 (2014).
Berry Rb, B. R. et al. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Version 2.4., (American Academy of Sleep Medicine, 2017).
Peppard, P. E. et al. Increased prevalence of sleep-disordered breathing in adults. Am. J. Epidemiol. 177, 1006–1014 (2013).
Heinzer, R. et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir. Med. 3, 310–318 (2015).
Nicholl, D. D. M. et al. Declining kidney function increases the prevalence of sleep apnea and nocturnal hypoxia. Chest 141, 1422–1430 (2012).
Lyons, O. D. et al. The effect of fluid overload on sleep apnoea severity in haemodialysis patients. Eur. Respir. J. 49, 1601789 (2017).
Roumelioti, M. E. et al. Sleep-disordered breathing and excessive daytime sleepiness in chronic kidney disease and hemodialysis. Clin. J. Am. Soc. Nephrol. 6, 986–994 (2011).
Sakaguchi, Y. et al. High prevalence of obstructive sleep apnea and its association with renal function among nondialysis chronic kidney disease patients in Japan: a cross-sectional study. Clin. J. Am. Soc. Nephrol. 6, 995–1000 (2011).
Donovan, L. M. & Kapur, V. K. Prevalence and characteristics of central compared to obstructive sleep apnea: analyses from the Sleep Heart Health Study cohort. Sleep 39, 1353–1359 (2016).
Nigam, G., Pathak, C. & Riaz, M. A systematic review of central sleep apnea in adult patients with chronic kidney disease. Sleep. Breath. 20, 957–964 (2016).
Unruh, M. L. et al. Sleep apnea in patients on conventional thrice-weekly hemodialysis: comparison with matched controls from the Sleep Heart Health Study. J. Am. Soc. Nephrol. 17, 3503–3509 (2006).
Beecroft, J. M., Pierratos, A. & Hanly, P. J. Clinical presentation of obstructive sleep apnea in patients with end-stage renal disease. J. Clin. Sleep. Med. 5, 115–121 (2009).
Weisbord, S. D. et al. Renal provider recognition of symptoms in patients on maintenance hemodialysis. Clin. J. Am. Soc. Nephrol. 2, 960–967 (2007).
Nicholl, D. D. et al. Diagnostic value of screening instruments for identifying obstructive sleep apnea in kidney failure. J. Clin. Sleep. Med. 9, 31–38 (2013).
Nicholl, D. D. et al. Clinical presentation of obstructive sleep apnea in patients with chronic kidney disease. J. Clin. Sleep. Med. 8, 381–387 (2012).
Sekercioglu, N., Curtis, B., Murphy, S. & Barrett, B. Sleep quality and its correlates in patients with chronic kidney disease: a cross-sectional design. Ren. Fail. 37, 757–762 (2015).
Unruh, M. L., Hartunian, M. G., Chapman, M. M. & Jaber, B. L. Sleep quality and clinical correlates in patients on maintenance dialysis. Clin. Nephrol. 59, 280–288 (2003).
Young, T. & Finn, L. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin Sleep Cohort. Sleep 31, 1071–1078 (2008).
Hla, K. & Young, T. Coronary heart disease incidence in sleep disordered breathing: the Wisconsin Sleep Cohort Study. Sleep 38, 677–684 (2015).
Marin, J. & Carrizo, S. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365, 1046–1053 (2005).
Gami, A. & Olson, E. Obstructive sleep apnea and the risk of sudden cardiac death: a longitudinal study of 10,701 adults. J. Am. Coll. Cardiol. 62, 610–616 (2013).
Gottlieb, D. & Yenokyan, G. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the Sleep Heart Health Study. Circulation 122, 352–360 (2010).
Shahar, E. & Whitney, C. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am. J. Respir. Crit. Care Med. 163, 19–25 (2001).
Bradley, D. & Floras, J. Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373, 82–93 (2009).
Xu, J., Yoon, I. Y. & Chin, H. J. The effect of sleep apnea on all-cause mortality in nondialyzed chronic kidney disease patients. Sleep. Med. 27-28, 32–38 (2016).
Tang, S. C. et al. Sleep apnea is a novel risk predictor of cardiovascular morbidity and death in patients receiving peritoneal dialysis. Kidney Int. 77, 1031–1038 (2010).
Harmon, R. R. et al. Obstructive sleep apnea is associated with interdialytic weight gain and increased long-term cardiovascular events in hemodialysis patients. Sleep. Breath. 22, 721–728 (2018).
Jhamb, M. et al. Association of sleep apnea with mortality in patients with advanced kidney disease. Clin. J. Am. Soc. Nephrol. 15, 182–190 (2020).
Sun, W. et al. Intermittent hypoxia-induced renal antioxidants and oxidative damage in male mice: hormetic dose response. Dose Response 11, 385–400 (2012).
Brooks, D., Horner, R. L., Kozar, L. F., Render-Teixeira, C. L. & Phillipson, E. A. Obstructive sleep apnea as a cause of systemic hypertension. Evidence from a canine model. J. Clin. Invest. 99, 106–109 (1997).
Horner, R. L., Brooks, D., Kozar, L. F., Tse, S. & Phillipson, E. A. Immediate effects of arousal from sleep on cardiac autonomic outflow in the absence of breathing in dogs. J. Appl. Physiol. 79, 151–162 (1995).
Somers, V. K., Dyken, M. E., Clary, M. P. & Abboud, F. M. Sympathetic neural mechanisms in obstructive sleep apnea. J. Clin. Invest. 96, 1897–1904 (1995).
Yokoe, T. et al. Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation 107, 1129–1134 (2003).
Ryan, S., Taylor, C. T. & McNicholas, W. T. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation 112, 2660–2667 (2005).
Dyugovskaya, L., Lavie, P. & Lavie, L. Increased adhesion molecules expression and production of reactive oxygen species in leukocytes of sleep apnea patients. Am. J. Respir. Crit. Care Med. 165, 934–939 (2002).
Zalucky, A. A. et al. Nocturnal hypoxemia severity and renin-angiotensin system activity in obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 192, 873–880 (2015).
Evans, R. G., Goddard, D., Eppel, G. A. & O’Connor, P. M. Factors that render the kidney susceptible to tissue hypoxia in hypoxemia. Am. J. Physiol. Regul. Integr. Comp. Physiol. 300, R931–940, (2011).
Abuyassin, B., Badran, M., Ayas, N. T. & Laher, I. Intermittent hypoxia causes histological kidney damage and increases growth factor expression in a mouse model of obstructive sleep apnea. PLoS One 13, e0192084 (2018).
Ahmed, S. B. et al. Nocturnal hypoxia and loss of kidney function. PLoS One 6, e19029 (2011).
Jaussent, I. et al. Impact of sleep disturbances on kidney function decline in the elderly. Eur. Respir. J. 47, 860–868 (2016).
Sakaguchi, Y. et al. Association of nocturnal hypoxemia with progression of CKD. Clin. J. Am. Soc. Nephrol. 8, 1502–1507 (2013).
Marrone, O. et al. Chronic kidney disease in European patients with obstructive sleep apnea: the ESADA cohort study. J. Sleep. Res. 25, 739–745 (2016).
Brenner, B. M., Meyer, T. W. & Hostetter, T. H. Dietary protein intake and the progressive nature of kidney disease: the role of hemodynamically mediated glomerular injury in the pathogenesis of progressive glomerular sclerosis in aging, renal ablation, and intrinsic renal disease. N. Engl. J. Med. 307, 652–659 (1982).
Fine, L. G., Orphanides, C. & Norman, J. T. Progressive renal disease: the chronic hypoxia hypothesis. Kidney Int. Suppl. 65, S74–S78 (1998).
Kraus, M. A. & Hamburger, R. J. Sleep apnea in renal failure. Adv. Perit. Dial. 13, 88–92 (1997).
Kimmel, P. L., Miller, G. & Mendelson, W. B. Sleep apnea syndrome in chronic renal disease. Am. J. Med. 86, 308–314 (1989).
Wadhwa, N. K., Seliger, M., Greenberg, H. E., Bergofsky, E. & Mendelson, W. B. Sleep related respiratory disorders in end-stage renal disease patients on peritoneal dialysis. Perit. Dial. Int. 12, 51–56 (1992).
Tada, T. et al. The predictors of central and obstructive sleep apnoea in haemodialysis patients. Nephrol. Dial. Transpl. 22, 1190–1197 (2007).
Boyd, J. H., Petrof, B. J., Hamid, Q., Fraser, R. & Kimoff, R. J. Upper airway muscle inflammation and denervation changes in obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 170, 541–546 (2004).
Brouns, R. & De Deyn, P. P. Neurological complications in renal failure: a review. Clin. Neurol. Neurosurg. 107, 1–16 (2004).
Tarasuik, A., Heimer, D. & Bark, H. Effect of chronic renal failure on skeletal and diaphragmatic muscle contraction. Am. Rev. Respir. Dis. 146, 1383–1388 (1992).
Elias, R. M. et al. Relationship of pharyngeal water content and jugular volume with severity of obstructive sleep apnea in renal failure. Nephrol. Dial. Transpl. 28, 937–944 (2013).
Elias, R. M., Bradley, T. D., Kasai, T., Motwani, S. S. & Chan, C. T. Rostral overnight fluid shift in end-stage renal disease: relationship with obstructive sleep apnea. Nephrol. Dial. Transpl. 27, 1569–1573 (2012).
Yumino, D. et al. Nocturnal rostral fluid shift: a unifying concept for the pathogenesis of obstructive and central sleep apnea in men with heart failure. Circulation 121, 1598–1605 (2010).
Anastassov, G. E. & Trieger, N. Edema in the upper airway in patients with obstructive sleep apnea syndrome. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 86, 644–647 (1998).
Arzt, M. & Eckert, D. J. Is fluid overload a target to treat sleep disordered breathing in patients with end-stage renal disease, and what are the underlying mechanisms? Eur. Respir. J. 49, 1700443 (2017).
Beecroft, J. et al. Enhanced chemo-responsiveness in patients with sleep apnoea and end-stage renal disease. Eur. Respir. J. 28, 151–158 (2006).
Beecroft, J. M. et al. Decreased chemosensitivity and improvement of sleep apnea by nocturnal hemodialysis. Sleep. Med. 10, 47–54 (2009).
Tanaka, A. et al. Factors associated with severity of sleep apnoea syndrome in patients with chronic kidney disease. Acta Cardiol. 72, 440–445 (2017).
Ogna, A. et al. Obstructive sleep apnea severity and overnight body fluid shift before and after hemodialysis. Clin. J. Am. Soc. Nephrol. 10, 1002–1010 (2015).
George, C. F. Reduction in motor vehicle collisions following treatment of sleep apnoea with nasal CPAP. Thorax 56, 508–512 (2001).
Jenkinson, C., Davies, R. J., Mullins, R. & Stradling, J. R. Comparison of therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised prospective parallel trial. Lancet 353, 2100–2105 (1999).
Nicholl, D. D. et al. Evaluation of continuous positive airway pressure therapy on renin-angiotensin system activity in obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 190, 572–580 (2014).
Nicholl, D. D. M. et al. Sex differences in renal hemodynamics and renin-angiotensin system activity post-CPAP therapy in humans with obstructive sleep apnea. Am. J. Physiol. Renal Physiol. 318, F25–f34 (2020).
Kinebuchi, S. et al. Short-term use of continuous positive airway pressure ameliorates glomerular hyperfiltration in patients with obstructive sleep apnoea syndrome. Clin. Sci. 107, 317–322 (2004).
Puckrin, R., Iqbal, S., Zidulka, A., Vasilevsky, M. & Barre, P. Renoprotective effects of continuous positive airway pressure in chronic kidney disease patients with sleep apnea. Int. Urol. Nephrol. 47, 1839–1845 (2015).
Chen, L. D. et al. Effect of positive airway pressure on glomerular filtration rate in patients with sleep-disordered breathing: a meta-analysis. Sleep. Breath. 21, 53–59 (2017).
Marrone, O. et al. Fixed but not autoadjusting positive airway pressure attenuates the time-dependent decline in glomerular filtration rate in patients with OSA. Chest 154, 326–334 (2018).
McEvoy, R. D. et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N. Engl. J. Med. 375, 919–931 (2016).
Loffler, K. A. et al. Effect of obstructive sleep apnea treatment on renal function in patients with cardiovascular disease. Am. J. Respir. Crit. Care Med. 196, 1456–1462 (2017).
Ahmed, S. B. Can treatment of obstructive sleep apnea with continuous positive airway pressure still improve kidney outcomes? Am. J. Respir. Crit. Care Med. 196, 1370–1371 (2017).
Rimke, A. N. et al. Effect of CPAP therapy on kidney function in patients with chronic kidney disease: a pilot randomized controlled trial. Chest 159, 2008–2019 (2021).
Tang, S. C. et al. Alleviation of sleep apnea in patients with chronic renal failure by nocturnal cycler-assisted peritoneal dialysis compared with conventional continuous ambulatory peritoneal dialysis. J. Am. Soc. Nephrol. 17, 2607–2616 (2006).
Kennedy, C., Ryan, S. A., Kane, T., Costello, R. W. & Conlon, P. J. The impact of change of renal replacement therapy modality on sleep quality in patients with end-stage renal disease: a systematic review and meta-analysis. J. Nephrol. 31, 61–70 (2018).
Tang, S. C. et al. Improvement in sleep apnea during nocturnal peritoneal dialysis is associated with reduced airway congestion and better uremic clearance. Clin. J. Am. Soc. Nephrol. 4, 410–418 (2009).
Lyons, O. D., Chan, C. T., Yadollahi, A. & Bradley, T. D. Effect of ultrafiltration on sleep apnea and sleep structure in patients with end-stage renal disease. Am. J. Respir. Crit. Care Med. 191, 1287–1294 (2015).
Beecroft, J. M., Zaltzman, J., Prasad, R., Meliton, G. & Hanly, P. J. Impact of kidney transplantation on sleep apnoea in patients with end-stage renal disease. Nephrol. Dial. Transpl. 22, 3028–3033 (2007).
Auckley, D. H., Schmidt-Nowara, W. & Brown, L. K. Reversal of sleep apnea hypopnea syndrome in end-stage renal disease after kidney transplantation. Am. J. Kidney Dis. 34, 739–744 (1999).
Lee, J. J. et al. Improvement of sleep-related breathing disorder in patients with end-stage renal disease after kidney transplantation. Clin. Transpl. 25, 126–130 (2011).
Forni Ogna, V. et al. Impact of kidney transplantation on sleep apnea severity: a prospective polysomnographic study. Am. J. Transpl. 20, 1659–1667 (2020).
Tandukar, S. et al. Does kidney transplantation affect sleep and fatigue in patients with kidney disease? Transplant. Direct 5, e461 (2019).
- The Renal Warrior Project. Join Now
- Source: https://www.nature.com/articles/s41581-024-00848-8
