Summary
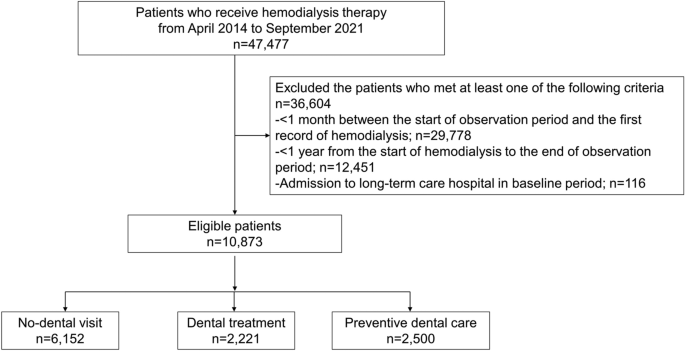
This study evaluated the effects of dental care utilization status in patients undergoing hemodialysis. Of the 10,873 patients undergoing hemodialysis extracted from a Japanese claims database, more than half had no-dental visits, 20.4% were in the dental treatment group and approximately 23.0% were in the preventive dental care group. The preventive dental care group had a lower incidence of CVD and infectious diseases. The HR of CVD was higher in the dental treatment group, whereas the HR of pneumonia was lower in the dental treatment group. These findings suggest that appropriate dental care utilization may be beneficial in reducing the risk of CVDs and infectious diseases, which are fatal complications in patients undergoing hemodialysis.
Comparison with previous studies
In the general population, periodontal disease is significantly associated with CVD16. A study using the national health insurance system database in South Korea has shown that severe periodontitis significantly increases the incidence of acute myocardial and cerebral infarctions17. However, no clear evidence of the preventive effects of periodontal therapy on the incidence of CVD events exist, although improvements in inflammatory markers and endothelial function have been reported18. Meanwhile, in patients undergoing hemodialysis with lower immune function and higher risk of developing CVD events compared with that observed in the general population, periodontal therapy may have a greater impact. In periodontal therapy for patients undergoing hemodialysis, several studies have elucidated the effect of controlling inflammation19,20,21 and preventing cardiovascular events22. Two studies using Taiwanese claims data reported that intensive periodontal therapy (scaling and root planing and flap procedure) lowered the risk of infection-related hospitalization13, hospitalization due to CVD, and all-cause mortality3 in patients undergoing hemodialysis.
However, multidisciplinary dental treatments may be provided in clinical practice because many patients who visit dentists suffer from various dental problems as well as periodontitis. Patients visiting dentists undergo two primary dental treatment modalities. Patients with dental problems should receive the active dental treatments for dental caries, endodontic treatment, tooth extraction, prosthodontic preparation, and intensive periodontal therapy. Patients without major dental problems may receive prophylaxis, including toothbrushing instructions, mechanical tooth polishing, scaling, root planing, and maintenance of the prosthodontic apparatus. This study focused on differences in patients’ dental care utilization patterns. No study has examined how multidisciplinary dental care, not only periodontal therapy, affects the prognosis of patients undergoing hemodialysis. In this study, patients who underwent nonsurgical periodontal therapy were assigned to the preventive dental care group because of its secondary preventive aspect. The results showed a significantly lower HR for the incidence of CVD and infectious diseases in the preventive dental care group were consistent with those of previous studies.
Possible explanations
Some possible mechanisms by which professional dental care affects CVD and infectious diseases in patients undergoing hemodialysis can be assumed, although detailed information on the participants, such as blood and bacteriological test results, were not available in this study. In general, the mechanisms by which oral health affects systemic health include the impact of local inflammation in the oral cavity due to dental diseases, systemic repercussions of the local inflammation through circulation, and influence of dental plaque containing abundant oral bacteria. In addition to these, specific mechanisms pertinent to patients undergoing dialysis may include the mediating effect of malnutrition–inflammation–atherosclerosis (MIA) syndrome.
Patients with periodontitis have systemic inflammation with raised levels of high-sensitivity C-reactive protein (CRP)23,24,25, and periodontal treatments reduce this inflammatory reaction19,20,21. A high CRP level is a decisive risk factor for CVD events26, and previous cohort studies have reported that the presence of periodontitis increases mortality from CVD in patients undergoing hemodialysis6,7. Therefore, well-achieved periodontal therapy has the potential to contribute to reducing the incidence of CVD. Regarding heart failure and cerebral infarction, a tendency toward reduced incidence risk was observed with preventive dental care, although no significant effects were found. CVDs are influenced by various factors including oral health, as well as lifestyle habits and environmental factors. Hence, this study’s sample size was likely insufficient to detect an impact of oral health.
In patients undergoing hemodialysis, the risks of infections including nosocomial infections are heightened. These risks are not only because these patients are immunocompromised but also because their rate of exposure to infection risks, such as hospitalizations, frequent outpatient visits27, and the placement of vascular access devices28, is high. Reducing the total number of bacteria in the oral cavity can help prevent infectious diseases. Poor oral health may increase the number of bacteria transferred into the bloodstream through daily oral activities such as tooth brushing and chewing29. These bacteria can trigger bacteremia and, eventually, sepsis in patients undergoing hemodialysis. However, in this study, dental care did not significantly reduce the risk of sepsis. Further larger-scale studies might detect the statistically significant effect of oral care on sepsis. Reducing the number of oral bacteria can prevent aspiration pneumonia30,31,32. Considering that patients undergoing hemodialysis are an immunocompromised population, preventive dental care may lower the incidence of pneumonia. Interestingly, a significantly lower incidence of pneumonia was observed not only in the preventive dental care group but also in the dental treatment group. Because we could not conduct stratified analyses for each type of dental treatment due to limited sample size, which specific dental treatments are associated with this lower incidence remains unclear. However, a reduction in oral bacterial load following caries treatment or extractions, professional denture cleaning33,34, or improved nutritional status through enhanced chewing efficiency following prosthodontic treatment35 could have enhanced immune responses. The additional analysis in this study suggests that major dental treatments involving pulpectomies, periodontal surgeries, or tooth extractions can be effective in reducing the risk of pneumonia.
Poor oral health may affect the incidence of CVD and infectious diseases through the MIA syndrome36,37. Some patients undergoing hemodialysis experience MIA syndrome, which is a combination of chronic systemic inflammation, malnutrition, and arteriosclerosis38. Oral problems, such as pain, ill-fitting dentures, and missing teeth with no prosthodontic treatment, may enhance malnutrition in patients undergoing hemodialysis patients39,40,41. Periodontitis increases systemic inflammation23,24,25. Malnutrition and inflammation proceed in a mutually conducive vicious cycle, leading to the risk of atherosclerosis and infections due to a depressed immune system in patients undergoing hemodialysis42.
Differences in the effects of dental treatments on the incidence of CVD and infectious diseases have been reported. The dental treatment visit group included people who visited for dental problems rather than for maintenance. The effect of poor oral health on the cardiovascular system before the baseline period may have been reflected in the significantly higher HR for CVD in the dental treatment group. The dental treatment group may represent a subpopulation with different health-related behaviors compared to the other groups, and this divergence in health-related behavior could potentially contribute to the observed results. In contrast, for pneumonia, when the number of oral bacteria is reduced by dental treatment, the effect may have been immediately apparent in the reduction in the risk of aspiration pneumonia.
Implications
In this study, a significant association was observed between preventive dental care and the incidence of CVD and infectious diseases. These findings suggest that preventive dental care, including prophylactic programs and maintenance of the prosthodontic apparatus, may be beneficial in patients undergoing hemodialysis. Oral care can reduce the risk of aspiration pneumonia in the older residents of nursing homes32, and that of cardiovascular diseases in the Scottish general population with a mean age of 50.0 years43. Patients undergoing hemodialysis are more susceptible to cardiovascular disease and infectious diseases, and have poor oral health. Therefore, the impact of dental utilization in our study population may have been more pronounced than in the general population. Effective prevention of CVD includes control of comorbidities, such as hypertension and conditions that cause inflammation, while prevention of infectious diseases includes primary infection control and vaccination. In addition, dental care may serve as a preventive measure. Patients undergoing hemodialysis have poor oral health44,45,46 because of salivary gland atrophy and drinking restrictions45. However, they were unlikely to visit dental clinics because of anxiety about dental treatment and financial concerns47,48. This study suggests that dental care provided by dental health professionals is beneficial for preventing fatal complications. Healthcare professionals should establish a system in which patients undergoing hemodialysis can receive preventive dental care without concern.
Dental visits, either dental treatment or preventive dental care, are associated with a lower risk of pneumonia, possibly owing to a reduction in oral bacteria. However, the finding that dental treatment is associated with a higher OR of the incidence of CVD needs to be examined in more detail in the future, including the type of treatment and the duration of time to CVD events.
Strength and limitations
To the best of our knowledge, this is the first study to demonstrate that regular dental visits may be beneficial in the primary prevention of CVDs and infectious diseases in patients with ESRD undergoing hemodialysis. Another strength of this study is that our longitudinal claims data included a large sample size without selection bias. Utilizing real-world data, we generated real-life clinical evidence for patients with ESRD undergoing hemodialysis.
However, this study also had several limitations. First, several potentially confounding factors, such as body mass index, smoking status, severity of periodontitis, unadjusted comorbidities that may affect physical activity, and socioeconomic status, were unavailable in the database. Regarding socioeconomic status, we adjusted for the type of health insurance as a proxy for income and educational background due to its correlation with income49. The data regarding income nor educational background were not available in the database used in this study. Second, our findings require careful interpretation for application to populations of different races or other dialysis modalities, such as peritoneal dialysis. Third, individuals without an observation period of 1 year after the initiation of hemodialysis were excluded in this study, potentially introducing survivor bias. This means artificially selecting a population with better health status, which may have led to an underestimation of the actual hazard ratios. Additionally, the no-dental visit group may include individuals who refrained from dental visits despite their poor oral health and those who refrained due to their good oral health. While this might be a potential bias, it may introduce variability in the results rather than skew them in a particular direction, thus ensuring the robustness of the study findings. Fourth, individuals were categorized into three groups based on their dental visit history during the baseline period, and each group was considered to exhibit a different dental utilization behavior. However, dental utilization behavior may change during the lifetime, and the potential effects of such changes require further investigation in future research. Furthermore, we did not account for dental visit behaviors prior to the baseline period. While the preventive dental care group may include individuals who received preventive dental care after undergoing significant dental procedures such as tooth extraction before the baseline period, we believe they are equivalent to those who continued preventive dental care without significant dental procedures prior to the baseline period, provided their oral health had improved by the start of the baseline period. Thus, to enhance the interpretability of the study findings, allocations were based solely on dental visit behaviors during the baseline period. Finally, the disease and procedure codes in the claims data were consistent. Previous studies that examined the validity of Japanese claims data demonstrated their usefulness in research using administrative data50,51,52. In Japan, no procedure code links directly to disease codes, leading to both dental treatments and preventive dental care being provided under the same disease codes. Therefore, exposure was defined based on dental procedure codes according to a previous study53.
- The Renal Warrior Project. Join Now
- Source: https://www.nature.com/articles/s41598-024-62735-3
