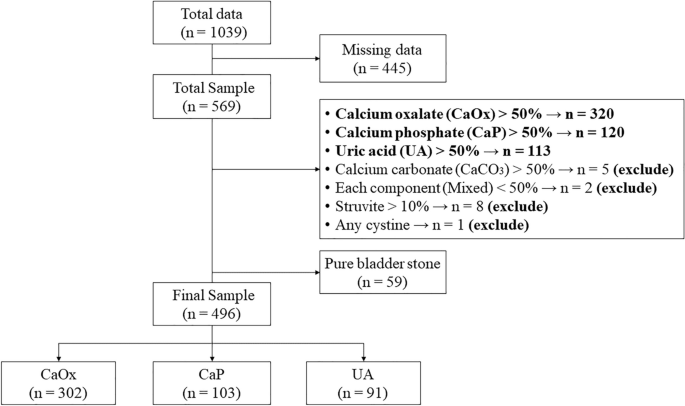
The incidence of bladder calculi has dramatically declined in recent years along with economic growth. Bladder calculi make up between 3% and 15% of all urinary stones in Asia8. Similar findings were found in our study, where bladder calculi accounted for about 10.4% of cases. Our study also revealed that CaOx stones were more frequently found in the upper urinary tract, while pure lower urinary tract stones were predominantly identified as UA stones. Additionally, the Chi-Square test demonstrated a significant difference between stone location and composition. This suggests that the etiologies of upper and lower urinary tract stones may vary, which was compatible with the previous study9. Consequently, we excluded pure lower urinary tract stones in this study.
Consistent with other studies, our research [Table 2] also identified CaOx as the most prevalent stone component, with a lower proportion compared to other Asian countries, while CaP had a relatively higher proportion. A research in an Asian population8 found that CaOx accounted for 75-90% of upper urinary tract stones, followed by UA (5-20%), CaP (6-13%), struvite (2-15%), apatite (1%), and cystine (0.5-1%).
In this study, a noticeable sex disparity was observed, with a male-to-female composition ratio of 1.99:1 [Table 2]. This finding is consistent with previous research conducted in Taiwan10, China11, and other Asian countries8. The higher occurrence of CaOx and UA stones in males may be attributed to the higher levels of androgens12 and lower urine pH, which have been shown to promote their formation. In the CaP groups, females were found to have a higher proportion than males. This could be attributed to the anatomical characteristics of females, which may make them more prone to urinary tract infections13, and be associated with alkaline urine.
Based on this study, urolithiasis is exceptionally rare in individuals below the age of 18 and beyond the age of 80. After reaching 18 years of age, the prevalence of urolithiasis steadily rises, peaking at 51–60-year-old middle-aged individuals, and then steadily declines, which is consistent with trends observed in most countries. As the predominant workforce in society, middle-aged individuals frequently participate in strenuous occupations, which can lead to unhealthy lifestyles characterized by irregular eating and sleeping patterns, insufficient fluid intake, sedentary behavior, and chronic occupational stress. The cumulative effect of these factors may elevate the risk of stone formation in middle-aged individuals. Consistent with the results in previous studies14, there is a trend of decreased proportion of CaOx stones with ageing. This trend may be associated with a decrease in urinary calcium excretion as individuals age15. Conversely, as patients aged, the proportion of UA stones rose, which was compatible with previous studies16. This could be related to the decline in renal function, urine pH and increased UA excretion in the elderly.
BMI is an indicator of obesity and is positively correlated with the risk of kidney stones, particularly in the production of UA and CaOx stones17. Adipose tissue in obese individuals releases pro-inflammatory and oxidative cytokines, exacerbating the relationship between obesity and kidney stone production by causing renal tissue damage and crystal deposition. UA stones are associated with factors like insulin resistance, renal fat deposition, and ammonia excretion defects. Dietary habits prevalent in obesity, such as high meat consumption, contribute to increased purine load and a reduction in urine pH, further elevating the risk of UA stone formation. Additionally, obesity elevates the risk of CaOx stones through heightened endogenous oxalate synthesis, increased intestinal absorption of oxalate, and elevated urinary oxalate excretion18. However, in our study, the findings for CaOx and UA stones showed no significant correlation, even when patients with a BMI > 25 were categorized as obese.
Hypertension is linked to increased calcium and oxalate excretion, heightened UA excretion in men, reduced citrate excretion, lower urine pH, and increased titratable acid excretion, contributing to a higher oversaturation of CaOx19. Several previous studies have found a higher incidence of UA stones among individuals with hypertension.
Type 2 DM has been recognized as a significant risk factor for kidney stone development, particularly UA stones16. Insulin resistance-induced hyperglycemia leads to the formation of advanced glycation end products (AGEs), triggering a pro-inflammatory response and causing vascular endothelial damage20. This condition not only decreases ammonium synthesis, leading to lower urine pH and an increased risk of UA stone formation but also elevates the risk of calcium stone formation by reducing urine citrate excretion21.
Dyslipidemia is associated with an elevated risk of kidney stones through various pathways, although the specific mechanisms contributing to this heightened risk remain undefined. Reduced levels of High-density lipoprotein (HDL) and elevated triglyceride (TG) levels, indicative of insufficient exercise and insulin resistance, are correlated with increased excretion of urinary sodium, oxalate, and UA, as well as a decrease in urine pH. These factors collectively elevate the likelihood of UA stone formation22. Additionally, heightened total cholesterol levels are significantly associated with increased urinary potassium and calcium excretion, potentially raising the risk of calcium stone formation.
Similarly to a previous study23, no significant relationship was found between the CaOx component and metabolic syndrome factors, even though these factors have been demonstrated to impact urinary levels of calcium, oxalate, and citrate. HTN, DM, and HLP were significantly linked to CaP and UA components in univariate analysis. Nevertheless, in multivariate analysis, only the association between CaP stones and DM remained negative. The aforementioned information confirms that metabolic syndrome factors as well as gout are correlated with low urinary pH, influencing the crystallization of both stone compositions, and resulting in differences in their composition.
Gout is a recognized risk factor for the formation of urinary stones24, particularly CaOx and UA stones. In patients with gout, uric acid stones are associated with a lower urinary pH, hyperuricemia and reduced fractional excretion of uric acid25. Moreover, inflammatory conditions and associated metabolic complications may elevate the risk of nephrolithiasis in patients with gout26. Aligning with prior study27, our research also indicated a significant positive relationship between gout and uric acid stones. Reducing urinary uric acid excretion with allopurinol has been shown to decrease the risk of CaOx stone formation28, and it alters the stone composition distribution in gout patients to resemble that of patients without gout. The lack of documented medication history for patients in our study might have influenced the absence of notable differences between the two groups.
Nephrolithiasis increases the risk of cardiovascular illnesses, especially coronary heart disease and stroke29, by being associated with atherosclerosis and vascular calcification. According to Ferraro et al.30, there is a connection between an increased risk of cardiovascular disease (CVD) and the concentration of CaP in stones. Bargagli et al.31 found that individuals with comorbid kidney stones and CVD tend to have reduced urinary excretion of citrate and magnesium, as well as a lower urine pH. Low urine citrate levels are frequently seen in those who develop CaP stones, and magnesium is essential for cardiovascular health and for preventing CaOx crystallization. Nevertheless, our study was consisted with earlier research, which did not discover a connection between stone composition and CVD31,32.
Studies conducted in Taiwan33 and the US34 showed that individuals with UA stones had much worse renal function than patients with CaP stones. Furthermore, patients with a lower estimated glomerular filtration rate (eGFR) exhibited a statistically significant correlation with reduced urinary pH, and a diminished urinary excretion of calcium and citrate. Li et al.35 also found a higher prevalence of CKD among patients with UA stones. It may be necessary to closely monitor renal function in patients with UA stones during follow-up. Our research indicated that UA stones have a significant positive correlation with CKD only in univariate regression analysis. The lack of detailed recording or documentation regarding CKD stages and biochemical indicators of renal function may have contributed to the observed differences in findings.
Prior research in southern Taiwan36 found that calcium urolithiasis development was independently influenced by current cigarette smoking, betel chewing, but not alcohol consumption. Smoking has been linked to an increased risk of urolithiasis due to its high concentration of toxic chemicals. Tobacco smoke has been found to elevate blood and kidney lead and cadmium levels, showing a positive association with CaOx stones and a negative association with UA stones37. It may also elevate vasopressin levels, exerting a strong vasoconstrictive effect, reducing urine output, and increasing the risk of urolithiasis. Additionally, it has been shown to be a separate risk factor for calcium urolithiasis, potentially contributing to the increased accumulation of calcium in the kidneys or reduced elimination of calcium through urine38. Smoking’s potential to release reactive oxygen species (ROS) may induce kidney damage and hasten the progression of chronic kidney disease, an acknowledged risk factor for lithogenesis. Moreover, smokers exhibit a lower incidence of UA stones compared to non-smokers, possibly attributed to reduced endogenous UA levels39, which may be linked to the antioxidant effect on ROS and free radicals produced by cigarettes and the depletion of antioxidants40. The precise effect of smoking on UA levels is still being debated. However, our study did not include the concentration of serum UA, so this aspect remains unknown. Despite no measurement of cadmium or lead concentrations, our study revealed that smoking negatively correlated with UA stones.
Consistent with our findings, urine pH significantly influences kidney stone formation. Most research indicates CaOx stones can form at any pH, with a consensus that their supersaturation is pH-independent. Conversely, CaP supersaturation rises rapidly with a urine pH above 6, particularly in the presence of hypercalciuria and hypocitraturia in alkaline urine41. As mentioned, UA stone formation might be attributed to aciduria, hyperuricosuria, or hyperuricemia, which could be caused by insulin resistance, altered purine metabolism, or impaired renal function. Among these factors, low urinary pH has been identified as having the most significant impact, resulting in reduced solubility of UA42. Decreased urine pH has been confirmed to be associated with BMI, metabolic factors, and HOMA-IR, which is a measure of insulin resistance.
Regarding study limitations, it is important to acknowledge that our stone analysis data were sourced from samples obtained during natural passage or surgery. The decision to submit samples for analysis relied on the discretion of the treating physician, lacking a standardized screening protocol, which could introduce bias. Additionally, the study’s reliance on data from a single medical center and the relatively small sample size may limit the generalizability of the findings to the broader population. Finally, the retrospective design could introduce data inaccuracies, and we did not collect comprehensive biochemical data such as serum calcium, phosphate, UA levels, or 24-hour urine analyses, as well as information on the history of medication use, which could influence stone formation. Despite its limitations, the study provides insights into urolithiasis characteristics, highlighting the need for larger, multicenter research to comprehensively understand the topic, possibly utilizing Taiwan’s National Health Insurance Research Database for diverse regional insights.
- The Renal Warrior Project. Join Now
- Source: https://www.nature.com/articles/s41598-024-64869-w
