In a retrospective cohort with 36 months of follow-up, we calculated patient eGFR from the collected data and plotted the trend of postoperative renal function. Moreover, we used multiple-factor regression analysis to evaluate the factors influencing the long-term progression of renal function. We also plotted curves depicting renal function changes in different patients and identified key nodes in their trajectories.
The poor progression of the patient’s long-term renal function after surgery was revealed, and the CKD grade increased. Studies have demonstrated that CKD after radical nephrectomy is associated with all-cause mortality and the incidence of cardiovascular disease [5]. Furthermore, after radical nephrectomy, patients choose different adjuvant therapies, such as chemotherapy, immunotherapy, and radiotherapy, according to the stage and grade of the tumour [9]. These treatments have specific requirements for renal function. Therefore, determining the factors influencing long-term renal function after surgery is crucial and necessitates the implementation of corresponding intervention measures in the early stages to prevent the occurrence of CKD.
Gender is an important factor influencing the occurrence of CKD, as shown by our data. Compared to women, men have a greater rate of all-cause and cardiovascular mortality, an increased risk of CKD progression, and a steeper decrease in the eGFR [7]. The reasons for potential sex-related differences in CKD progression are unclear, but differences in potential risk factors and sex hormone effects have been proposed [10]; for example, animal studies have shown a protective, anti-inflammatory effect of oestrogen on podocytes and a reduced permeability effect on the glomerular endothelium [11, 12].
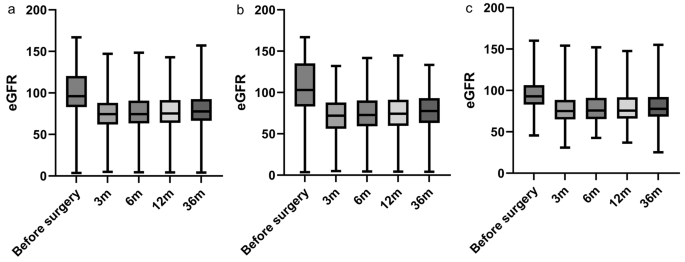
Research has proven that radical nephrectomy gradually restores renal function in patients [2, 13]. Figures 1 and 2 show that the renal function of most patients decreased after surgery. Our research also revealed that in most patients, postoperative renal function gradually declined within 3 months of surgery and remained stable after 3 months. Subsequently, the renal function of most patients gradually stabilized 3 months after surgery. For most patients, the long-term trajectory of renal function can be reasonably predicted based on the renal function observed at the 3-month mark after surgery. Additionally, one study demonstrated that 49% of patients recovered their preoperative eGFR within 2 years of radical nephrectomy for renal cell carcinoma [14]. Therefore, we believe that 3 months after surgery is the period during which renal function is most likely to be impacted, and the protection of renal function at this stage is crucial.
The box plots of eGFR at different time points. m = month a: eGFR of all patients at different time periods. b: eGFR of patients who don’t experienced AKI at different time periods c: eGFR of patients who experienced AKI at different time periods
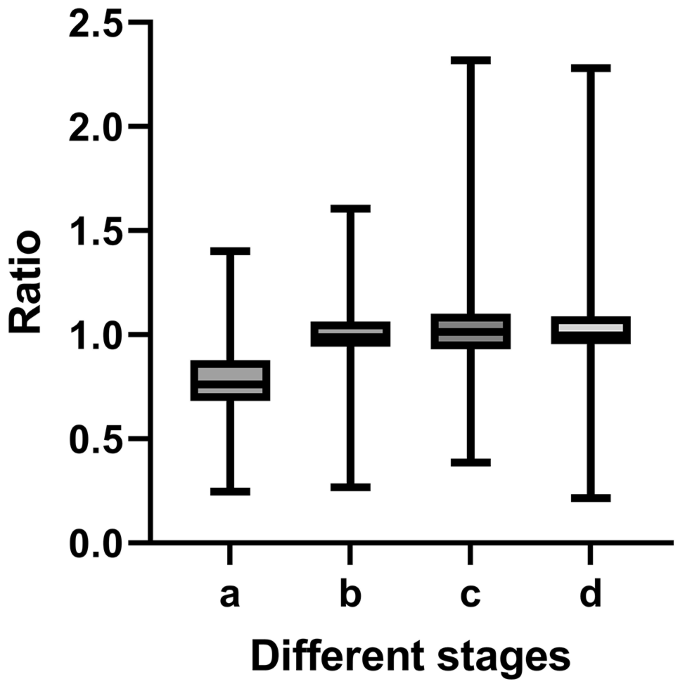
The rate of change at different stages. a: The ratio of the 3-month eGFR to the preoperative eGFR. b: The ratio of the 6-month eGFR to the 3-month eGFR. c: The ratio of the 12-month eGFR to 6-month eGFR. d: The ratio of the 36-month eGFR to the 12-month eGFR
In addition, Table 3 shows that the most important factor for long-term renal function was the rate of change in the eGFR during the early postoperative period. During this period, owing to the removal of the affected kidney, the contralateral healthy kidney compensates with hyperplasia, thus supplying the entire body [15]. Therefore, the kidney remaining during this period is extremely fragile owing to the workload. According to the Remnant Kidney Model, after the reduction of kidney mass, the workload for the remaining nephrons results in progressive renal damage leading to terminal renal failure [16]. Therefore, healthy kidneys may undergo permanent changes during this time, with important implications for long-term kidney function. This is also reflected in the data obtained in our study. During this period, the influence of the rate of change in the eGFR on long-term renal function surpassed that of age, and it subsequently stabilized. Hence, this period represents the optimal time for predicting and safeguarding renal function.
Several studies have demonstrated that postoperative AKI is a common complication after radical nephrectomy [17, 18]. According to a literature review, 41–47% of patients develop clinical AKI within 48 h after radical nephrectomy [19], consistent with the incidence of AKI reported in our cohort. Some studies have suggested that postoperative AKI after radical nephrectomy is associated with the deterioration of long-term renal function [20, 21].
In our research, we studied the relationship between the ratio of postoperative creatinine to preoperative creatinine and the rate of change in renal function 3 months after surgery. The greater the ratio, the more severe the degree of AKI [8]. Therefore, AKI can be used as an indicator of short-term postoperative renal function, and the compensatory capacity of the kidney can be used to further predict long-term renal function.
However, we believe that postoperative AKI after radical resection differs from postoperative AKI in other typical clinical situations. In other typical clinical cases, postoperative AKI refers to the destruction of the renal parenchyma and reduction of glomeruli caused by ischaemia, inflammation, and immune factors [22, 23]. Hypotensive shock-induced AKI mainly occurs in clinical situations such as cardiovascular surgery and kidney transplantation. The pathogenesis is primarily ischemia-reperfusion injury, leading to renal hypoxia-ischemia necrosis and long-term fibrosis [24]. he causes of AKI are numerous, among which, renal ischemia-reperfusion injury caused by perioperative hypotension is a significant factor leading to AKI and can result in long-term renal function decline. However, data from this study indicate that perioperative hypotension is not a risk factor for CKD, which may be related to the lower incidence of hypotensive shock in our data. The development of postoperative AKI after radical nephrectomy does not damage the contralateral healthy kidney and prompts compensatory hyperplasia in the remaining kidney [25]. Immediately after nephrectomy, a 40% increase in blood flow and the GFR was observed in the kidneys [26]. This progresses to affect the glomeruli, increasing the high-pressure experienced by the nephron filters and resulting in compensatory enlargement of the glomeruli [25].
Once the glomerular volume reaches a certain threshold, glomerulosclerosis, hypertension, proteinuria, and renal failure may occur [27]. An increase in renal blood flow and the GFR leads to increased oxygen consumption, which in turn leads to tissue hypoxia. These conditions induce hypoxia-inducible Factor 1α and vascular endothelial growth factor. Hypoxia also induces small tube phosphatases and tension homologues, leading to tubular regeneration and repair [28]. Therefore, serum creatinine levels rapidly increase after unilateral nephrectomy, leading to AKI. To confirm that postoperative creatinine may be attributed exclusively to nephrectomy without damage to the contralateral kidney, AKI markers should be introduced into clinical practice to quantify any suffering of the contralateral kidney [19, 29].
The occurrence and severity of AKI after nephrectomy can be used as detection indicators, enabling more informed assessments and the formulation of programs aimed at enhancing short-term renal function recovery. These strategies include reducing the prerenal load, controlling blood pressure, and eating properly. Moreover, they contribute to long-term renal function. The recent literature revealed remaining kidney parenchymal (contralateral kidney) could predict the new baseline eGFR. It could be a tool for decision choice of treatment for the RCC patients [30]. Further studies are needed.
However, this study has the following limitations that need to be addressed in future research. First, it should further expand the sample size for follow-up and include novel biomarkers of AKI, cystatin C and/or NephroCheck test [19, 29]. Secondly, due to the inconvenience of clinical sample collection, urinary volume is not included in the diagnostic criteria for AKI.
Conclusion.
In conclusion, postoperative renal function in most patients gradually declined within 3 months of surgery and remained stable after 3 months. More attention should be given to AKI patients during the first 3 postoperative months, especially for those with decreased renal function. Additionally, the implementation of appropriate measures is very important for the recovery of patients with long-term renal function impairment. These measures can also help when deciding to adopt treatment options that may be highly demanding in terms of renal function.
- The Renal Warrior Project. Join Now
- Source: https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-024-03601-2