Written by: Beth Dougherty
.posted-on a[rel=”bookmark”] { display: none; }
Prostate cancer is the most common cancer diagnosed in men. When found early, before it has spread, patients can do extremely well.
However, prostate cancer risks vary due to genetics, health care access, socioeconomics, and environmental exposures. Some groups have higher risks and worse outcomes. For example:
- Black men have a rate of death from prostate cancer that is more than double those of every other racial group.
- In addition, Black men, particularly men of West African descent, are nearly twice as likely to be diagnosed with prostate cancer than Caucasian men and three times more likely than Asian men.
The best way to improve your chances of a good outcome is to detect prostate cancer early, which is possible with screening.
“We have a really well-defined screening test, the prostate specific antigen (PSA) test, that is just a blood draw,” says Stephanie Berg, DO, a medical oncologist in the Lank Center for Genitourinary Oncology. “It can be extremely accurate. In the case of an elevated PSA, we have more tools available today than ever before that can be used to rule out or diagnose prostate cancer.”
Prostate cancer screening recommendations emphasize personal decision-making with the help of your doctor. Here are five things you need to know to help you understand your prostate cancer risk and actively participate in decision-making about prostate cancer screening.
1. Learn the screening recommendations.
Prostate cancer screening is appropriate for anyone with a prostate, including cisgender men, trans women, non-binary people, and other gender nonconforming people who were assigned male at birth or who have a prostate.

According to the American Urological Association:
- Patients and their doctors should engage in “shared decision-making” about prostate cancer screening. Your role as a patient is to inform your doctor of your family history and share your personal preferences. Together you can decide if screening is right for you.
- Screening typically begins between ages 45 and 50. For those at a higher risk, including people with African ancestry or a family history, screening should begin between ages 40 and 45.
If you are in your 40s or 50s and are experiencing any urinary concerns or unexplained, new back pain, talk to your doctor about prostate cancer screening.
Prostate cancer screening is considered preventive medicine and should be covered by insurance plans. If you do not have insurance, free or low-cost screening may be available near you. Search the ZeroCancer database or the US Health Resources and Services Administration database for options.
2. Learn about your family’s history of prostate cancer.
Your prostate cancer risk goes up if you have a close blood relative – a sibling, a parent, a parent’s sibling, or a grandparent – who had prostate cancer.
The only way to know about your family’s history of prostate cancer is to talk about it. Not all families and cultures have a tradition of sharing information about cancer with one another, but in the case of prostate cancer, it is important to know as much as possible. Any family history suggests you might be at a higher risk and might consider screening at an earlier age than someone with an average risk.
If anyone in your family has experienced aggressive prostate cancer, diagnosis of the disease before age 65, or diagnosis after the cancer has spread, you might be at an even higher risk of prostate cancer and might consider screening even earlier than someone of high risk.
3. Learn about your family’s history of breast, ovarian, or pancreatic cancer.
Some families have an elevated risk of breast, ovarian, pancreatic, and prostate cancer because they carry one or more of the BRCA and other related genes that increase the chances of these cancers. These genes occur in every cell in the body and can be passed from a parent to a child the same way hair color or eye color are passed down.
When thinking about your personal risk of prostate cancer, it is important to consider the experiences of your sisters, mother, aunts, and grandmothers with breast or ovarian cancer, if possible, and the experiences of any close relative with pancreatic cancer.
If you have a family history of these diseases, tell your doctor. You might also consider screening earlier than someone of average risk for prostate cancer.
4. Be an active participant in your decisions about screening.
Screening for prostate cancer is done using a blood test that determines your level of prostate-specific antigen (PSA). An elevated level beyond the normal range requires more investigation.
An elevated PSA is not a definitive indicator of prostate cancer. A slight elevation beyond the normal range might be normal for an individual. A significant elevation will likely be treated by a doctor with more urgency.


In the past, doctors frequently performed biopsies of the prostate to diagnose cancer after an elevated PSA test. But today, there are many other tests that can be done first to determine if a biopsy is necessary. Those tests may include:
- Digital rectal exam
- Another PSA test
- Testing another biological marker in the blood
- Imaging such as ultrasound or MRI
Learn more about how we diagnose prostate cancer at Dana-Farber.
5. Know what to expect if you receive a prostate cancer diagnosis.
Treatment for prostate cancer that has not spread is typically provided by a urologist. Many factors are considered when choosing the best treatment plan.
For some patients, active surveillance, with more frequent monitoring for signs of disease, is the best option. Others might be treated with surgery, radiation, or hormone therapy depending on the specifics of their case.
Learn more about how we treat prostate cancer at Dana-Farber.
About the Medical Reviewer
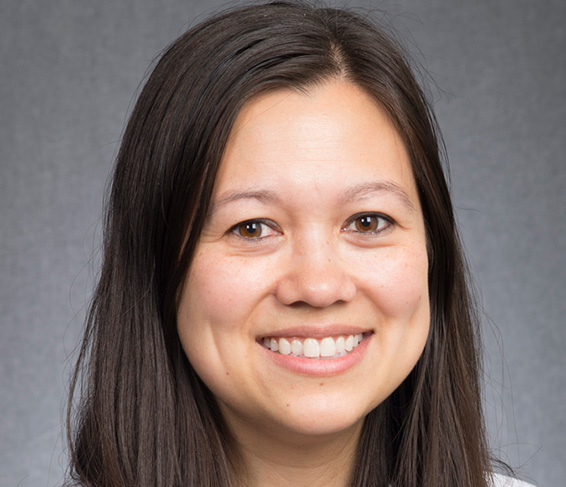
Dr. Stephanie Berg is a medical oncologist for the Lank Center of Genitourinary Oncology. She completed her medical education at the Lake Erie College of Osteopathic Medicine. Her post-graduate training in Internal Medicine was completed at the University of Illinois-Chicago where she served as Chief Resident and hematology-oncology fellowship at Loyola University Medical Center where she served as Chief Fellow. She was an Assistant Professor of Medicine at Loyola University Chicago in the Department of Medicine and Cancer Biology from 2018-2022. Prior to her arrival at Dana-Farber Cancer Institute, she was the junior faculty lead of the Genitourinary Medical Oncology Program at the Cardinal Bernardin Cancer Center of Loyola University Chicago. She was also the research head of Renal Cell Cancer clinical trials and served as the principal investigator on several cooperative group and industry sponsored trials. Her aim is to be at the forefront of translating basic science research to better understand the pathogenesis of cancer development, participate in novel gene discovery and identify potential molecular therapeutic targets for future genitourinary cancer treatment. She has a special interest in older adult oncology and novel immunotherapy drug development.
- The Renal Warrior Project. Join Now
- Source: https://blog.dana-farber.org/insight/2024/05/prostate-cancer-risk-and-screening-five-things-you-need-to-know/
