Study population
The prospective observational and cohort study was performed including two groups of patients with ESRD undergoing replacement therapy with hemodialysis (HD) from two different Nephrology Units of the Southern and Norther Italy. The first group of 16 HD patients was enrolled at the Nephrology Dialysis and Transplantation Unit of the University Hospital “Ospedali Riuniti”, Foggia (Italy) and was used as main cohort (Testing Group). The second group of 36 HD patients was enrolled at the Nephrology Dialysis and Transplantation Unit of the University of Eastern Piedmont “Amedeo Avogadro”, Novara (Italy) and was used to validate the results obtained in the testing group of patients (Validation Group).
All the enrolled patients were > 18 and < 80 years old and COVID-19 naïve. Exclusion criteria were: therapy with immunosuppressive drugs, previous kidney transplant, systemic infections, cancer, HIV positivity or other life-threatening conditions with life expectancy lower than 6 months.
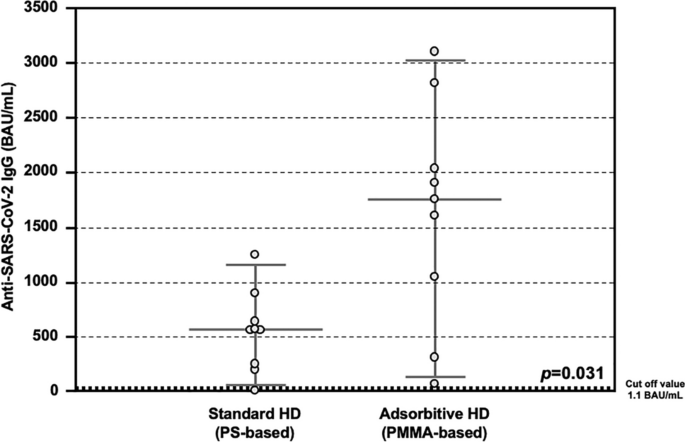
This study aimed to compare the immunomodulatory effects of adsorptive dialytic treatments (Poly-methyl-methacrylate or PMMA-based) on COVID vaccine response compared to conventional Polysulphone-based dialytic treatments. Nevertheless, a limited number of patient chronically treated with PMMA membranes entering the inclusion criteria were followed at two different Nephrology Units involved in the study (26 HD patients). For this reason, a propensity-score matching analysis was conducted in R using the MatchIt package with nearest-neighbor 1-to-1 matching to compare HD patients treated with PMMA with HD patients treated with conventional dialytic membrane (Polysulfone).
All the enrolled patients were treated thrice a week with hemodialysis (HD) treatment for at least 12 months. Both in the Testing Group [TG] and in the Validation Group [VG], half of the patients were treated with maintenance PMMA-based HD (AdsorptiveAdsorptive HD or AHD; n = 8 for [TG] and n = 18 for [VG], respectively) and the remaining with maintenance conventional HD with Polysulphone (PS) (Standard HD or SHD; n = 8 for [TG] and n = 18 for [VG], respectively).
Low-molecular weight or unfractionated heparin was administered as standard anti-coagulation therapy. Dialysis prescription was guided aiming at a value of urea reduction rate ≥ 0.65 and a Kt/V ≥ 1.2. The above parameters of dialysis adequacy were calculated according to the second-generation Daugirdas equation31.
To rule out the possibility of active or previous SARS-CoV-2 infection, all the patients of both groups were assessed for both PCR nasal swab and detection of anti-SARS-CoV-2 IgM and IgG, both resulted negative, and were therefore considered as SARS-CoV-2 naïve.
The two study groups were enrolled from each separate hospital. Several meetings before the study initiation were made to confirm the absence of difference on dialysis condition (water quality or COVID19 infection status) between the two dialytic centers.
After signing an informed consent to participate to the present study, all the enrolled patients received two doses of the anti-SARS-CoV-2 mRNA BNT16b2 Vaccine (Comirnaty, Pfizer-Biontech, USA). All the clinical data at enrolment were collected and recorded.
The study protocol conformed to the ethical guidelines of the Declaration of Helsinki and was approved by the institutional review board (Decision no. 1570/2021 of 04 April 2021; Ethical Committee at the University Hospital “Policlinico Riuniti” of Foggia). This was in accordance with the guidelines laid down by the Regional Ethics Committee on human experimentation.
Sample collection
In all the enrolled subjects of both the groups, serum samples were collected before vaccination (Time 0, T0) and fourteen days after the second vaccine dose (Time 2, T2) and stored at − 30 °C, until analyzed.
Only in the enrolled subjects of the Testing Group, whole blood (25 ml) was collected from all patients at T0 and T2, as previously described32. Peripheral blood mononuclear cells (PBMCs) were isolated by density separation on SepMateTM (STEMCELL Technologies, Vancouver, Canada), according to manufacturer’s instructions, and stored at − 80 °C, until analyzed.
Detection of anti SARS-CoV-2 antibodies
Anti-SARS-CoV-2 Ig were titrated in both Testing Group and Validation Group two week after the second dose of vaccine with different methods, according to the local laboratory protocols.
In detail, as previously described32, anti-SARS-CoV-2 IgG and IgM titre in the Testing Group was analyzed by using a chemiluminescent analytical assay (CLIA) commercially available kit (New Industries Biomedical Engineering Co., Ltd [Snibe], Shenzhen, China), according to the manufacturer instructions. Reagent wells were coated with recombinant structural protein CoV-S (spike) and e CoV-N (nucleocapside) of SARS-CoV-2 for both IgM and IgG assay. For IgM assay, the microspheres were coated with a monoclonal antibody to capture human IgM followed by the addition of recombinant antigen from virus 2019-nCoV marked with amino-butylethyl-isoluminol (ABEI). The samples, serum or plasma, were diluted by instrument. The relative light units (RLU) detected was proportional to the concentration of IgG/M in sample. An RLU-ratio of the measurement of each sample to the supplied calibrator was calculated. According to manufacturer instructions, IgG assay BAU/mL of < 1 was considered negative, 1.0–1.1 borderline and > 1.1 positive; for IgM, an BAU/mL < 0.9 was considered negative, 0.9 to 1.0 borderline and > 1.0 positive. Clinical sensitivity was estimated by the manufacturer as 78.65% and 91.21% for IgM and IgG, respectively, while specificity was estimated as 97.50% and 97.3% for IgM and IgG, respectively.
Anti-SARS-CoV-2 IgG titre in the Validation Group was analyzed with a quantitative method for detection of IgG antibodies against the S1-RBD antigen (Atellica IM SARS-CoV-2 IgG [sCOV2G], Siemens Healthineers, Erlangen, Germany). This test is a fully automated, 2-step sandwich immunoassay, with indirect chemiluminescent technology. The patient specimen is incubated with preformed complex of streptavidin-coated particles and biotinylated SARS-CoV-2 recombinant antigens. The antibody-antigen complex is detected by an acridinium ester–labeled antihuman IgG mouse mAb. According to manufacturer instruction, IgG assay > 1.00 was considered positive. Clinical sensitivity for IgG was estimated by the manufacturer as 96.41%, while specificity was estimated as 99.90%.
Neutralizing antibodies levels assessment
Only in the enrolled subjects of the Testing Group, serum neutralizing antibodies (NAb) levels were assayed, using a commercially available ELISA Kit, according to the manufacturer’s instructions (SARS-CoV-2 NeutraLISA, EUROIMMUN Medizinische Labor diagnostika AG, Lübeck, Germany), as previously described32. This competitive semi-quantitative test allows to evaluate the ability of Nab to prevent the link between the S1/RBD domain and the ACE2 receptor. In detail, microplate was coated with recombinant S1/RBD domain of SARS-CoV-2. Sample and controls were diluted 1:5 in dilution buffer containing soluble ACE2 conjugated to biotin and incubated in the reaction wells. Both Nab and soluble ACE2 competed for the binding site on the antigen surface. The photometric measurement at 450 nm yielded the results as a percentage of inhibition (%IH). According to manufacturer instructions, 20%IH was considered negative, 20 to 35%IH borderline and > 35%IH positive.
Interferon-gamma release assay (IGRA)
Only in the enrolled subjects of the Testing Group, PBMCs isolated from patients were thawed, counted and stimulated with SARS-CoV-2 IGRA stimulation tube set (EUROIMMUN Medizinische Labor diagnostika AG, Lübeck, Germany), as previously described32.
In details, 1*106 PBMCs were resuspended in PBS/EDTA and dispensed in each of the three stimulation tubes for 20 h: CoV-2 IGRA BLANK for the determination of the background concentration of IFNy; CoV-2 IGRA STIM containing a mitogen causing non-specific secretion of IFNy; CoV-2 IGRA TUBE containing SARS-CoV-2 S1 components for the determination of specific IFNy secretion. After stimulation, samples were centrifuged and the supernatants used for subsequent quantitative assay using IFNy ELISA, according to the manufacturer instructions (EUROIMMUN Medizinische Labor diagnostika AG, Lübeck, Germany). Reaction wells were coated with anti-IFNy monoclonal antibody. Samples and controls were diluted 1:5 in a diluent buffer, incubated and processed according to manufacturer instructions. For IFNy quantification a 4-parameters logistics was applied.
Statistical analysis
Statistical analysis was performed using SPSS 25.0 software (IBM Corp., Armonk, NY. Variable distribution was tested using Kolmogorov–Smirnov test. Serum parameters were compared between groups by Student’s t-test for unpaired data and Mann–Whitney U-test, as appropriate. Frequencies were compared among groups by F-Fisher or X2-test, as appropriate. Correlation between two variables was ascertained by Pearson or Spearman’s correlation tests, as appropriate. All the data are reported as mean ± standard deviation (SD), median and interquartile range (IQR), or as percentage frequency, unless otherwise specified. A p-value < 0.05 was considered statistically significant.
- The Renal Warrior Project. Join Now
- Source: https://www.nature.com/articles/s41598-024-62044-9
