Shivam Joshi, MD, is an adjunct Clinical Assistant Professor of Medicine at the NYU Grossman School of Medicine and practices at the Orlando VA Medical Center. He has a research interest in plant-based diets in kidney disease and has authored or co-authored dozens of peer-reviewed articles. He speaks frequently on this subject to audiences worldwide, and is the youngest nephrologist to receive the highest award in renal nutrition, the National Kidney Foundation’s Joel D. Kopple Award. You can follow him on Twitter, Instagram (@sjoshiMD), and on his website (www.afternoonrounds.com).
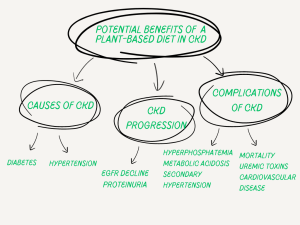
There has recently been an uptick in the adoption of plant-based diets for lifestyle diseases like diabetes, obesity, primary hypertension, and heart disease. However, plant foods were historically excluded from the “renal diet” of yesteryear due to a medley of concerns, like hyperphosphatemia, hyperkalemia, and protein deficiency – none of which were supported by the literature. As such, there is now a growing interest in the diet and its potential application for patients with kidney disease. Plant-based diets have many benefits in kidney disease beyond reducing the risk of developing CKD or CKD progression, including potentially treating the causes and complications of kidney disease (Figure 1).
In this wave of emerging research, we have the study by Amir et al. recently published in AJKD examining the association between adherence to plant-based diets and the risks of CKD and all-cause mortality of 2,539 participants with CKD in the Chronic Renal Insufficiency Cohort (CRIC). The study further separated plant-based diets into overall plant-based diets, healthy plant-based diets, and unhealthy plant-based diets. This is important as plant-based diets can be unhealthy. For example, a person can be ‘plant-based’ but may be subsisting on white bread, fries, chips, and candy. This is not healthy and not recommended by credible health professionals. Returning to the study by Amir et al., it is best to discuss the two outcomes individually.
In terms of the outcome of CKD progression, Amir et al. did not find a statistically significant association between the tertiles of any of the plant-based diets and CKD progression. Although this finding is not isolated, it is not the end of the story. A meta-analysis by Kelly et al. also found no association between healthy dietary patterns and the risk of end-stage kidney disease (ESKD) among adults with CKD. However, this meta-analysis included only 3 studies for its analysis on CKD progression and had several other limitations, including not having a score for plant-based diets specifically. Since the publication of this meta-analysis, new evidence has emerged showing otherwise. Notably, the Singapore Chinese Health Study made headlines for following over 63,000 participants over a median of 15.5 years and finding a dose-dependent association with red meat intake and kidney failure. Studies by Bernier-Jean et al. and Knight et al. have demonstrated similar findings, especially in women. When looking at other outcomes, like prevalent or incident CKD, there are nearly a dozen other prospective and cross-sectional studies showing a beneficial association with plant foods. Returning to the study by Amir et al., one reason they may not have found an association is the small differences in plant food consumption between the tertiles. Looking at Table 2 of their study, the fiber consumption was 8, 10.1, and 12.2 g/d for tertiles 1, 2, and 3, respectively. For fruit consumption, the values were 0.88, 1.23, and 1.79 servings per day for tertiles 1, 2, and 3 respectively. Although these differences were statistically significant, they were not clinically significant due to the low consumption of fiber and plant foods even in the highest tertile. For example, the recommended fiber consumption, including for those with kidney disease, is 25 grams of fiber per day for women and 38 grams for men. In CRIC, those in the highest tertile were consuming less than half the recommended fiber intake. One reason for the low plant food consumption may be the active discouragement of plant foods by members of the renal community for the aforementioned reasons (hyperphosphatemia, hyperkalemia, and protein deficiency). CRIC’s enrollment occurred in the mid 2000s and participants were followed until 2018, which is around the time when the renal community started to rethink its position on plant foods. Lastly, in the continuous analysis by Amir et al., a 10-point higher score for the unhealthy plant-based index was associated with a 14% higher risk of CKD progression. Others, notably Kim et al. using the ARIC (Atherosclerosis Risk in Communities Study) cohort, have also showed an association with an unhealthy plant-based diet and adverse renal outcomes. This is not surprising as unhealthy plant foods are – after all – unhealthy.
Turning our attention to the outcome of all-cause mortality, Amir et al. found that participants with the highest vs. lowest adherence to an overall plant-based diet and a healthy plant-based diet had a 26% (HR 0.74) and a 21% (HR 0.79) lower risk of all-cause mortality, respectively. This is both surprising and unsurprising at the same time. Given the lack of a beneficial finding seen with the prior outcome, one could suspect that no association would also be seen here given the low consumption of plant food intake. However, other studies, including those by Chen et al. and Gutierrez et al., have demonstrated similar findings. One reason for the signal is that fiber may be a mediator of mortality in CKD as it has been shown to be associated with reduced mortality and cardiovascular disease in CKD. In one study, every extra gram of fiber was linked to a 11% reduction in cardiovascular events. Fiber may exert its benefits through a number of ways, including a reduced dietary acid load in the associated food, more saccharolytic fermentation (and less proteolytic fermentation), and being packaged with antioxidants, to name a few. There may be other benefits beyond fiber, including indirect benefits of plant foods with the underlying causes of kidney disease, e.g. diabetes and hypertension.
In the end, although Amir et al. did not show that plant foods helped reduce the risk of CKD progression, but they did show that an unhealthy plant-based diet was associated with a higher risk of CKD progression and all-cause mortality. A cohort that consumed more plant foods might have allowed for more separation in events between the tertiles to show a possible benefit of plant foods with reduced CKD progression. Nonetheless, this important study adds to the growing literature and will hopefully spur much needed randomized controlled trials on this issue.
– Post prepared by Shivam Joshi @sjoshiMD
To view Amir et al [FREE], please visit AJKD.org.
Title: Adherence to Plant-Based Diets and Risk of CKD Progression and All-Cause Mortality: Findings From the Chronic Renal Insufficiency Cohort (CRIC) Study
Authors: Saira Amir, Hyunju Kim, Emily A. Hu, Ana C. Ricardo, Katherine T. Mills, Jiang He, Michael J. Fischer, Nishigandha Pradhan, Thida C. Tan, Sankar D. Navaneethan, Mirela Dobre, Cheryl A.M. Anderson, Lawrence J. Appel, and Casey M. Rebholz on behalf of the CRIC Study Investigators
DOI: 10.1053/j.ajkd.2023.09.020
- The Renal Warrior Project. Join Now
- Source: https://ajkdblog.org/2024/06/27/plants-kidney-disease-and-mortality-evidence-from-cric/