Patient characteristics
We identified 6,996 patients with incident HF (5,149 with HFpEF and 1,847 with HFrEF) (See Table 1). At baseline, patients who developed HFpEF tended to be older, more often female, and more commonly had atrial fibrillation, anemia, COPD, hypertension, liver disease, and cancer, while those who developed HFrEF had higher prevalence of coronary artery disease and prior myocardial infarction (MI). Baseline eGFR was similar between both groups.
Exposure
An AKI event occurred during the ascertainment period in 6.9% of those who developed HFpEF and 5.7% of those who developed HFrEF (see Table 2). The overall distribution of AKI severity was higher among those who developed HFrEF (61%, 20%, and 19% for stages 1, 2, and 3, respectively) versus HFpEF (72%, 16%, and 13% for stages 1, 2, and 3, respectively, P = 0.062) though the difference was not statistically significant.
Outcomes
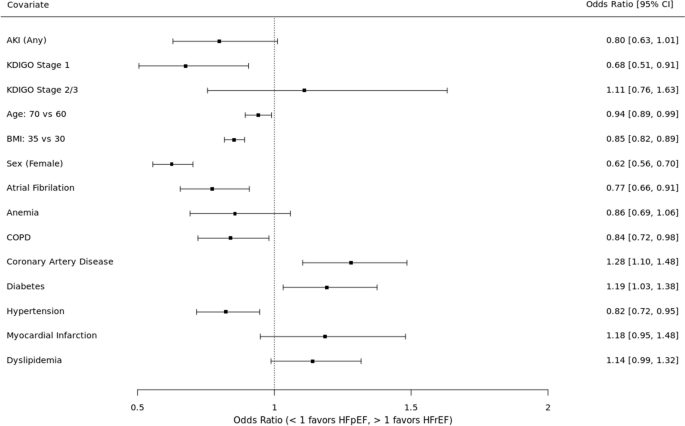
See Fig. 3. In the unadjusted analysis, AKI was not preferentially associated with HF subtype (OR 0.81, 95% CI 0.65 – 1.02). When examined by AKI severity, stage 1 AKI was associated with 31% higher odds of HFpEF (OR 0.69, 95% CI 0.52 – 0.92) whereas stage 2–3 had a non-significant trend towards HFrEF (OR 1.12, 95% CI 0.77 – 1.61).
Risk of HFpEF versus HFrEF. Results of primary analysis. Odds ratios for each covariate indicate higher odds of HFpEF (OR < 1) or HFrEF (OR > 1)
In the adjusted analysis, AKI trended toward an association with HFpEF (OR 0.80, 95% CI 0.63 – 1.01) but did not meet statistical significance. When examined by AKI severity, stage 1 AKI was associated with 32% higher odds of HFpEF (OR 0.68, 95% CI 0.51 – 0.91) whereas stage 2–3 had a non-significant trend towards HFrEF (OR 1.11, 95% CI 0.76 – 1.63). The covariates with statistically significant associations with HFpEF included older age, higher BMI, female sex, atrial fibrillation, and hypertension. The covariates with significant associations with HFrEF included coronary artery disease and black race.
Sensitivity analyses
HF defined by diagnosis code + BNP + diuretic
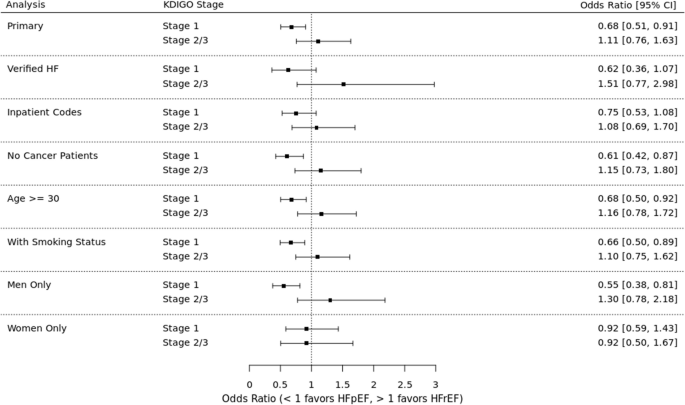
See Fig. 4 for sensitivity analyses results. Among patients for whom BNP and diuretic data were available, AKI (all stages) was associated with 13% higher odds of HFpEF (OR 0.87, 95% CI 0.56 – 1.33). Stage 1 AKI was associated with 38% higher odds of HFpEF (OR 0.62, 95% CI 0.36 – 1.07) and stage 2–3 AKI was associated with 51% higher odds of HFrEF (OR 1.51, 95% CI 0.77 – 2.98).
Risks of HFpEF versus HFrEF in primary analysis and sensitivity analyses. Odds ratios for each analysis indicate higher odds of HFpEF (OR < 1) or HFrEF (OR > 1)
HF defined by only inpatient diagnosis code
Among patients in whom HF was diagnosed by an inpatient diagnosis code, AKI (all stages) was associated with 14% higher odds of HFpEF (OR 0.86, 95% CI 0.64 – 1.14). Stage 1 AKI was associated with 25% higher odds of HFpEF (OR 0.75, 95% CI 0.53 – 1.08) and stage 2–3 AKI was associated with 8% higher odds of HFrEF (OR 1.08, 95% CI 0.69 – 1.70).
Patients without cancer
Among patients without a history of cancer, AKI (all stages) was associated with 24% higher odds of HFpEF (OR 0.76, 95% CI 0.57 – 1.01). Stage 1 AKI was associated with 39% higher odds of HFpEF (OR 0.61, 95% CI 0.42 – 0.87) and stage 2–3 AKI was associated with 15% higher odds of HFrEF (OR 1.15, 95% CI 0.73 – 1.80).
Patients > 30 years of age
Among patients aged 30 years or older, AKI (all stages) was associated with 19% higher odds of HFpEF (OR 0.81, 95% CI 0.63 – 1.03). Stage 1 AKI was associated with 32% higher odds of HFpEF (OR 0.68, 95% CI 0.50 – 0.92) and stage 2–3 AKI was associated with 16% higher odds of HFrEF (OR 1.16, 95% CI 0.78 – 1.72).
Including imputed smoking status
In this analysis that used imputed data for smoking status, AKI (all stages) was associated with 21% higher odds of HFpEF (OR 0.79, 95% CI 0.62 – 1.00). Stage 1 AKI was associated with 34% higher odds of HFpEF (OR 0.66, 95% CI 0.50 – 0.89) and stage 2–3 AKI was associated with 10% higher odds of HFrEF (OR 1.10, 95% CI 0.75 – 1.62).
Excluding patients with HF with mildly reduced EF (HFmrEF)
In this analysis that was limited to patients with EF < 40% or ≥ 50%, AKI (all stages) was associated with 22% higher odds of HFpEF (OR 0.78, 95% CI 0.60 – 1.03). Stage 1 AKI was associated with 39% higher odds of HFpEF (OR 0.61, 95% CI 0.43 – 0.87) and stage 2–3 AKI was associated with 25% higher odds of HFrEF (OR 1.25, 95% CI 0.81 – 1.92).
Analysis stratified by sex
To evaluate for differences in outcomes by sex, we first replicated the primary analysis in each sex. Among men, AKI (all stages) was associated with 27% higher odds of HFpEF (OR 0.73, 95% CI 0.53 – 0.99). Stage 1 AKI was associated with 45% higher odds of HFpEF (OR 0.55, 95% CI 0.38 – 0.81), while stage 2–3 AKI was associated with 30% higher odds of HFrEF (OR 1.30, 95% CI 0.78 – 2.18). Among women, AKI (all stages) was associated with 8% higher odds of HFpEF (OR 0.92, 95% CI 0.64 – 1.32). Stage 1 and stages 2–3 AKI were both associated with 8% higher odds of HFpEF (stage 1 OR 0.92, 95% CI 0.59 – 1.43; stage 2–3 OR 0.92, 95% CI 0.50 – 1.67.) We included a sex-by-AKI interaction term in the model to evaluate for effect modification by sex, which was not statistically significant.
Analysis of weighted cohort
As an additional sensitivity analysis, we used inverse probability of treatment weights (IPTW) to synthesize a cohort that could match the HFrEF patients to the HFpEF on all observed covariates except for AKI, as would be done in a case–control study with a sufficient number of controls to allow such matching. Characteristics of the weighted cohort are detailed in Table 3. In this analysis, AKI (all stages) was associated with 20% higher odds of HFpEF (OR 0.80, 95% CI 0.60 – 1.05). Stage 1 AKI was associated with 33% higher odds of HFpEF (OR 0.67, 95% CI 0.48 – 0.93) and stage 2–3 AKI was associated with 14% higher odds of HFrEF (OR 1.14, 95% CI 0.72 – 1.82).
Post hoc analysis
Given the unexpected opposite directionality of the point estimates for stage 1 AKI compared to stages 2–3 AKI, we conducted a post hoc analysis to test for a unique additional effect of severe AKI in contrast to the overall AKI effect. In this analysis, the overall AKI effect (all AKI stages) was associated with 32% higher odds of HFpEF (OR 0.68, 95% CI 0.51 – 0.91), while the additional severe AKI effect (stage 2–3 AKI) was associated with 64% higher odds of HFrEF which was statistically significant (OR 1.64, 95% CI 1.03 – 2.63).
We also examined the number of MI events in each group to determine if a larger proportion of MIs during or after stage 2–3 AKI could explain the risk of HFrEF. Of the 460 patients with AKI, 39 had an MI (defined by presence of both a diagnosis code for myocardial infarction and elevated troponin level) during or within 5 days of the AKI hospitalization; of these, 31 developed HFpEF and 8 developed HFrEF. Similarly, 25% of those with stage 1 AKI and 20% of those with stage 2–3 AKI had an MI in the time between the AKI event and the date of HF.
- The Renal Warrior Project. Join Now
- Source: https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-024-03602-1