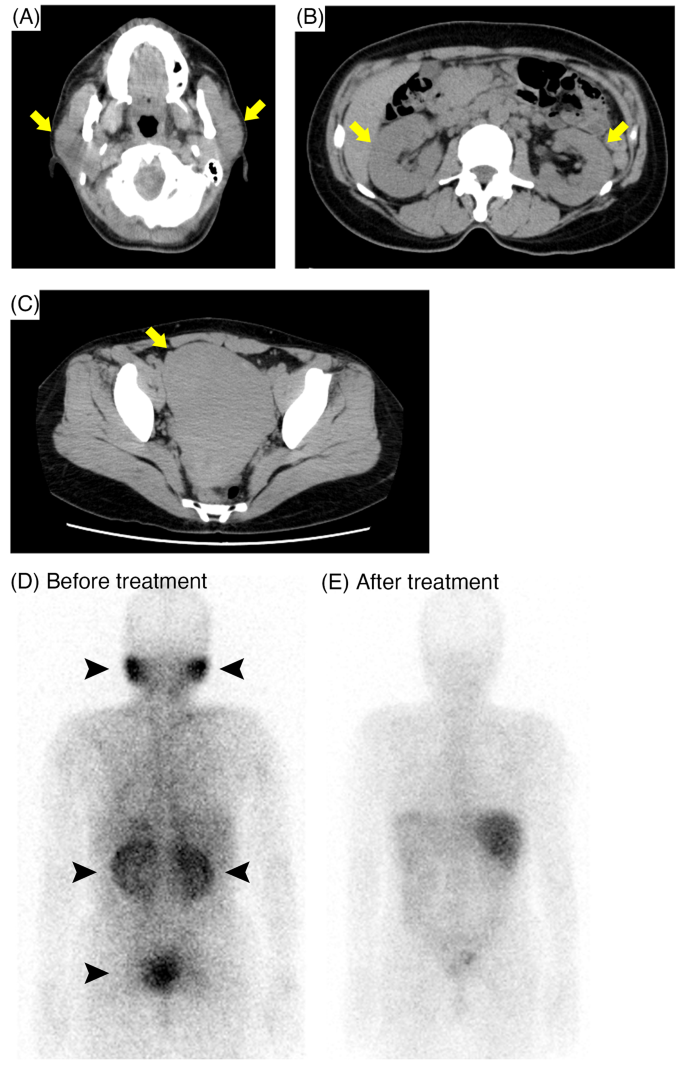
A 51-year-old Japanese female was referred to our hospital with bilateral parotid swelling and renal dysfunction. There was no previous medical history of renal dysfunction. Physical examination revealed bilateral parotid swelling and lower legs edema. She also presented hypermenorrhea. Laboratory findings showed elevated levels of serum creatinine 3.1 mg/dL, serum corrected calcium 10.6 mg/dL, angiotensin converting enzyme (ACE) 44.9 U/L (reference range 8.3–21.4 U/L), and lysozyme 75 µg/mL (reference range 5.0–10.2 µg/mL). The urinary β2-microglobulin (β2-MG) level was also elevated (Table 1). Computed tomography (CT) scan revealed swelling of bilateral kidneys, parotid glands, and uterus (Fig. 1A, B, C, respectively). Additionally, Ga scintigraphy showed remarkable accumulation in these organs (Fig. 1D). Ocular screening was performed but uveitis was not indicated.
Findings of Computed tomography (CT) scan and Ga scintigraphy. (A, B, C) CT scan showed swelling of parotid glands (A), bilateral kidneys (B), and uterus (C, arrows). (D) Ga scintigraphy before treatment showed remarkable accumulation in these organs (arrowheads). (E) After the treatment, the accumulation has disappeared
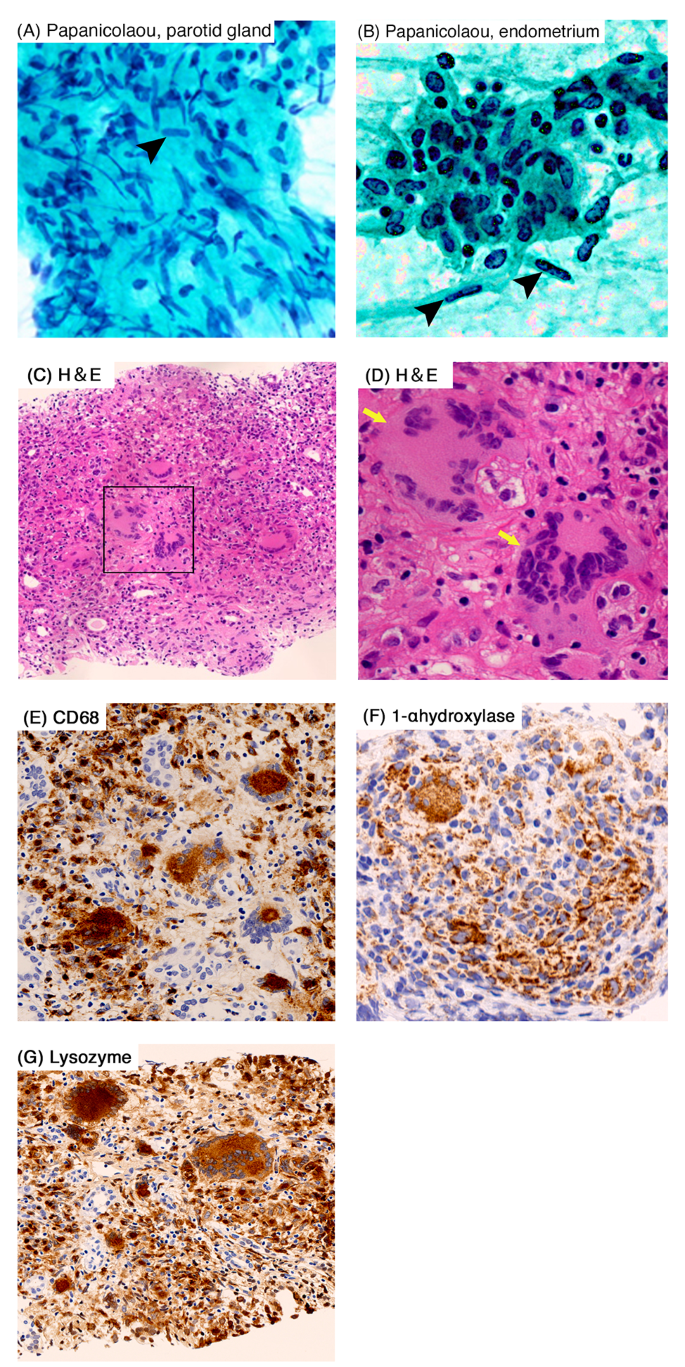
After admission, the needle aspiration cytology of parotid gland, endometrial cytology and renal biopsy were performed, respectively. Both parotid gland and endometrial cytology showed the presence of epithelioid cells indicating sarcoidosis (Fig. 2A, B, respectively). In the renal biopsy, light microscopy showed tubulointerstitial nephritis with diffuse non-caseating epithelioid cell granulomas and presence of diffuse multinucleated giant cells (Fig. 2C and D). A significant infiltration of inflammatory cells was observed in the interstitial area and around the renal tubules, with positive staining for CD68 (Fig. 2E), a specific marker of macrophages. Due to the presence of hypercalcemia and increased lysozyme level, we also performed 1-α hydroxylase (CYP27B1) and lysozyme staining. Both staining showed remarkable positivity in multinucleated giant cells and infiltrating cells (Fig. 2F, G, respectively). No notable findings were observed in the glomeruli, and all immune-fluorescence staining were negative.
Cytologic findings of parotid gland and endometrium, and light microscopic findings of the renal biopsy. (A and B) Papanicolaou staining showed the presence of epithelioid cells in parotid gland (A) and endometrium (B). (C and D) Hematoxylin and eosin staining (H&E) showed the tubulointerstitial nephritis with diffuse non-caseating epithelioid cell granulomas and diffuse multinucleated giant cells (arrows). (E) Inflammatory cells and multinucleated giant cells showed positive in CD68 staining. (F and G) 1-α hydroxylase (F) and lysozyme staining (G) were positive in inflammatory cells and multinucleated giant cells. Original magnification, ×400 (A, B, D), x100 (C), ×200 (E, F, G), respectively
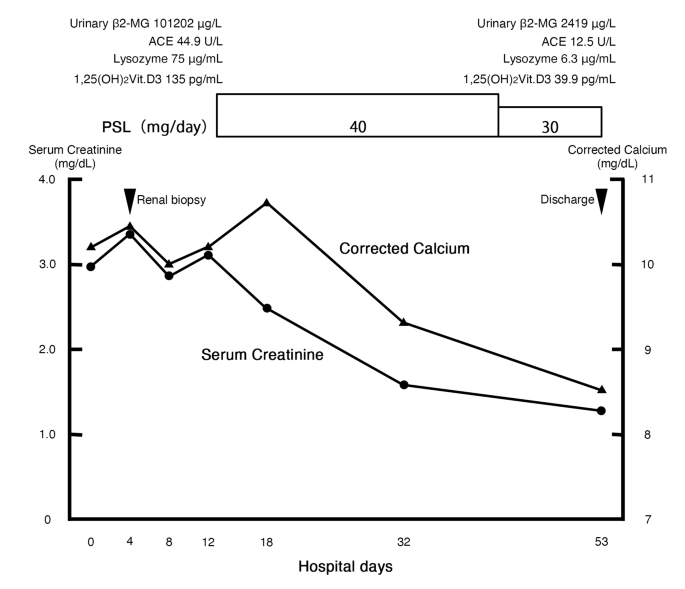
Based on the pathological findings, we diagnosed as renal sarcoidosis complicated by parotid glands and uterine lesions. As a treatment, prednisolone was initiated at a dose of 40 mg/day (0.8 mg/kg/day) since the 11th day, resulting in rapid improvement of renal function and hypercalcemia (Fig. 3). Furthermore, levels of urinary β2-MG, serum ACE, serum lysozyme, and serum 1,25(OH)2 vitamin D3 decreased. After the treatment, second Ga scintigraphy was performed, and the accumulation in the kidneys, parotid glands and uterus was disappeared (Fig. 1E). On the 53th day, the patient discharged.
Clinical course after admission. ACE, angiotensin converting enzyme; β2-MG, β2-microglobulin; PSL, prednisolone
After the discharge, the patient’s condition is stable without the apparent recurrence and serum ACE levels are also maintained within the normal range from 7.2 to 18.4 U/L for at least 30 months.
- The Renal Warrior Project. Join Now
- Source: https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-024-03635-6